Jambo!
Ready for another great day at Lewa. We started with our circuit training session outside overlooking the savannah of Northern Kenya. It’s a healthy beginning to our morning and in keeping with our message of prevention of Chronic Disease.
After our breakfast we take our short ride to the clinic breathing in the fresh air and smells of nature. We arrive to the big smile of Rosaline (of course) as well as patients who are already waiting at the clinic for the afternoon clinic hours with the Naweza doctors.
But before we see the patients, we have a full morning of presentations by our doctors as well as Benard, the lead on our Kenyan research studies.
The topics included were:
- Benard – Findings from the CVD Program
- Kristen – Type 1 Diabetes
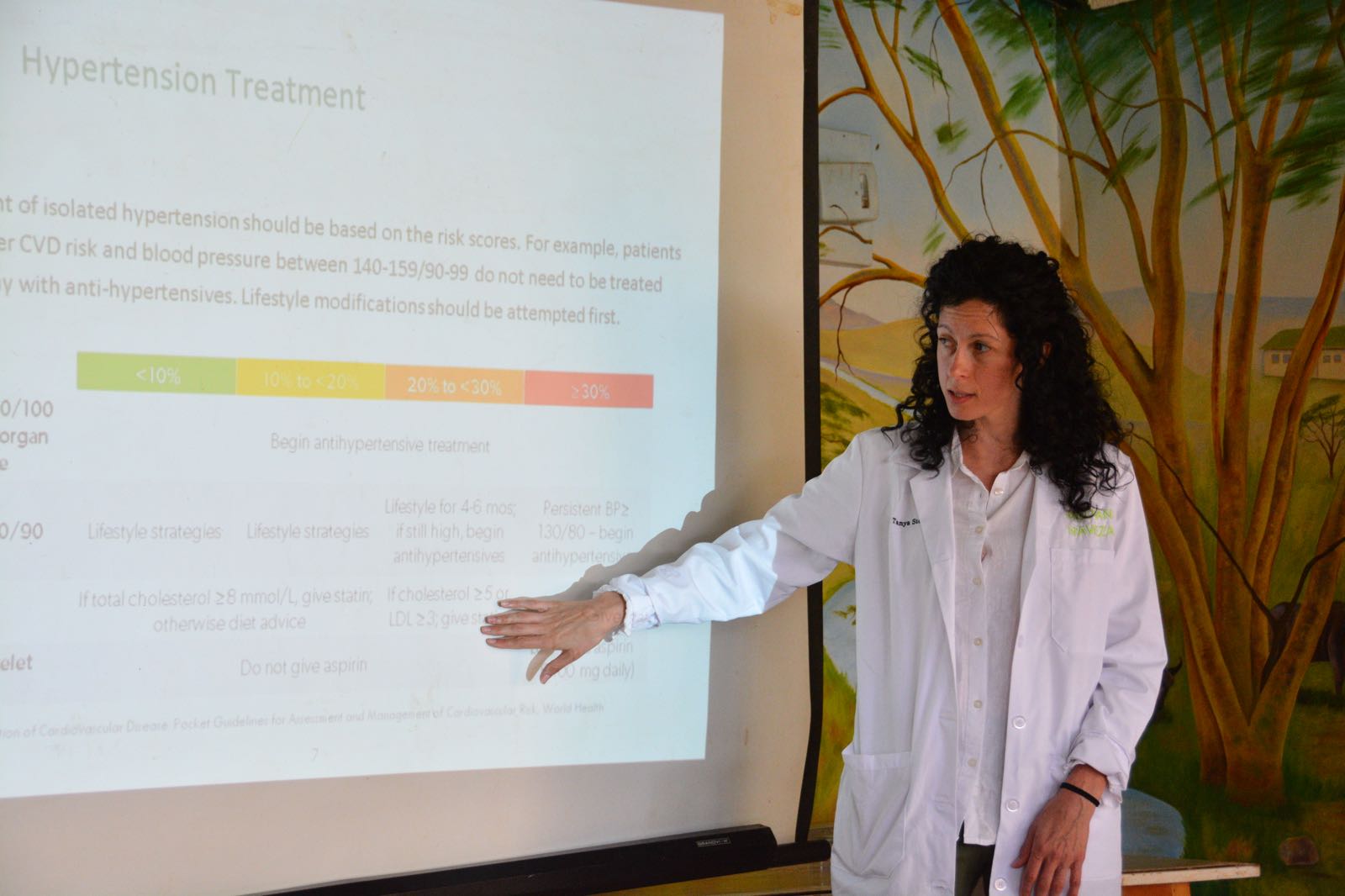
- Dr. Tanya – Diabetes and Hypertension Review + Post CVD Event Care
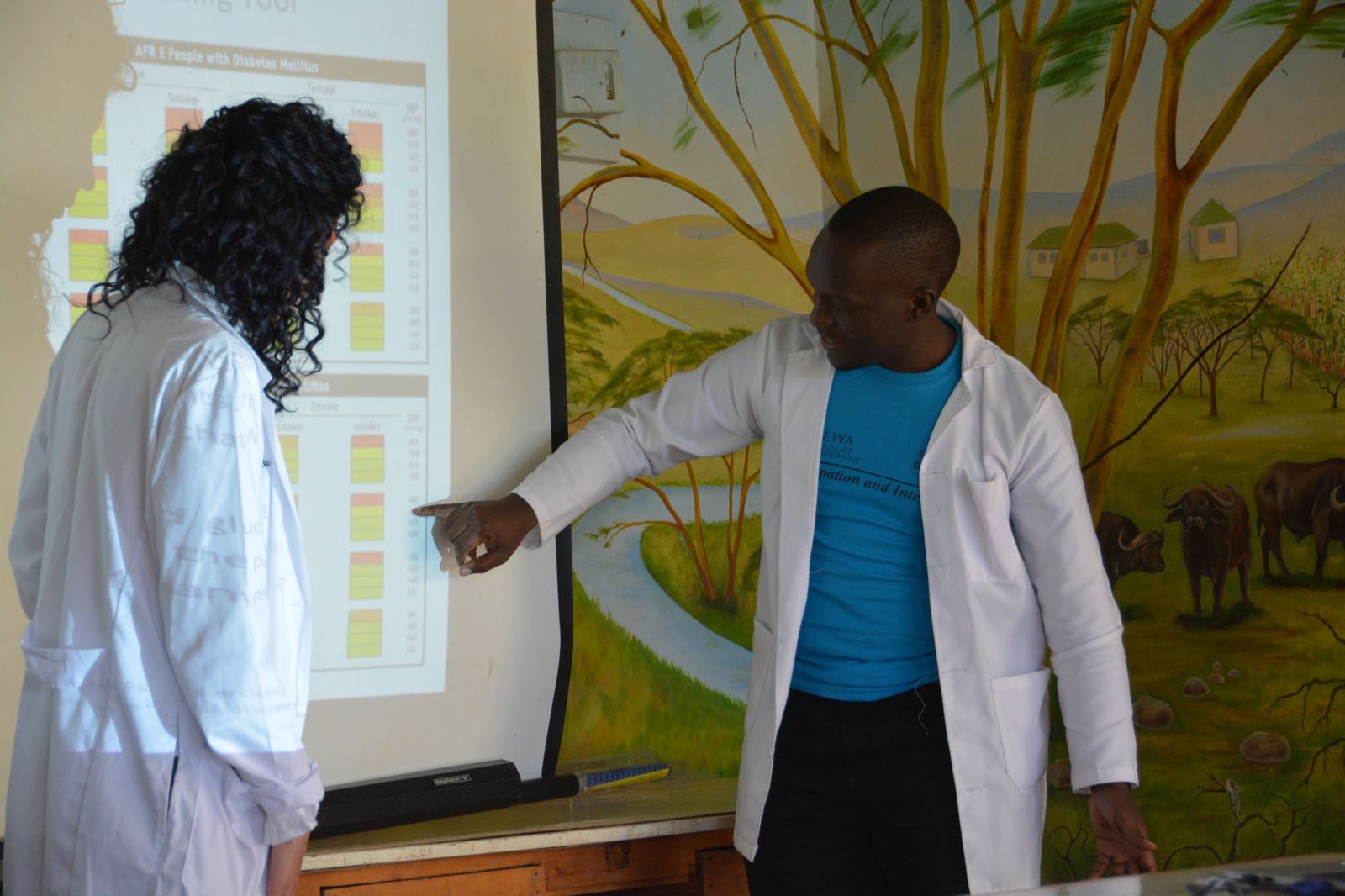
Benard gave an excellent summary of our CVD program study so far. The study will provide proof-of-concept that a community health worker, equipped with a novel “mHealth” technology on her cell phone, can screen for hypertension and diabetes in the community setting. Non-communicable diseases are increasing in importance globally, and these “silent killers” contribute to cardiovascular disease (heart attack and stroke) which are now overtaking infectious diseases as the leading causes of death. Our study is an innovative strategy for active case-finding in a rural setting, in order to identify patients in need of lifestyle and pharmacologic interventions to reduce the risk of cardiovascular disease. By subjecting our program to the scrutiny of a scientific study, we are applying a high level of rigour to our clinical activities, and we will be able to report our findings to the scientific community for potential scalability.
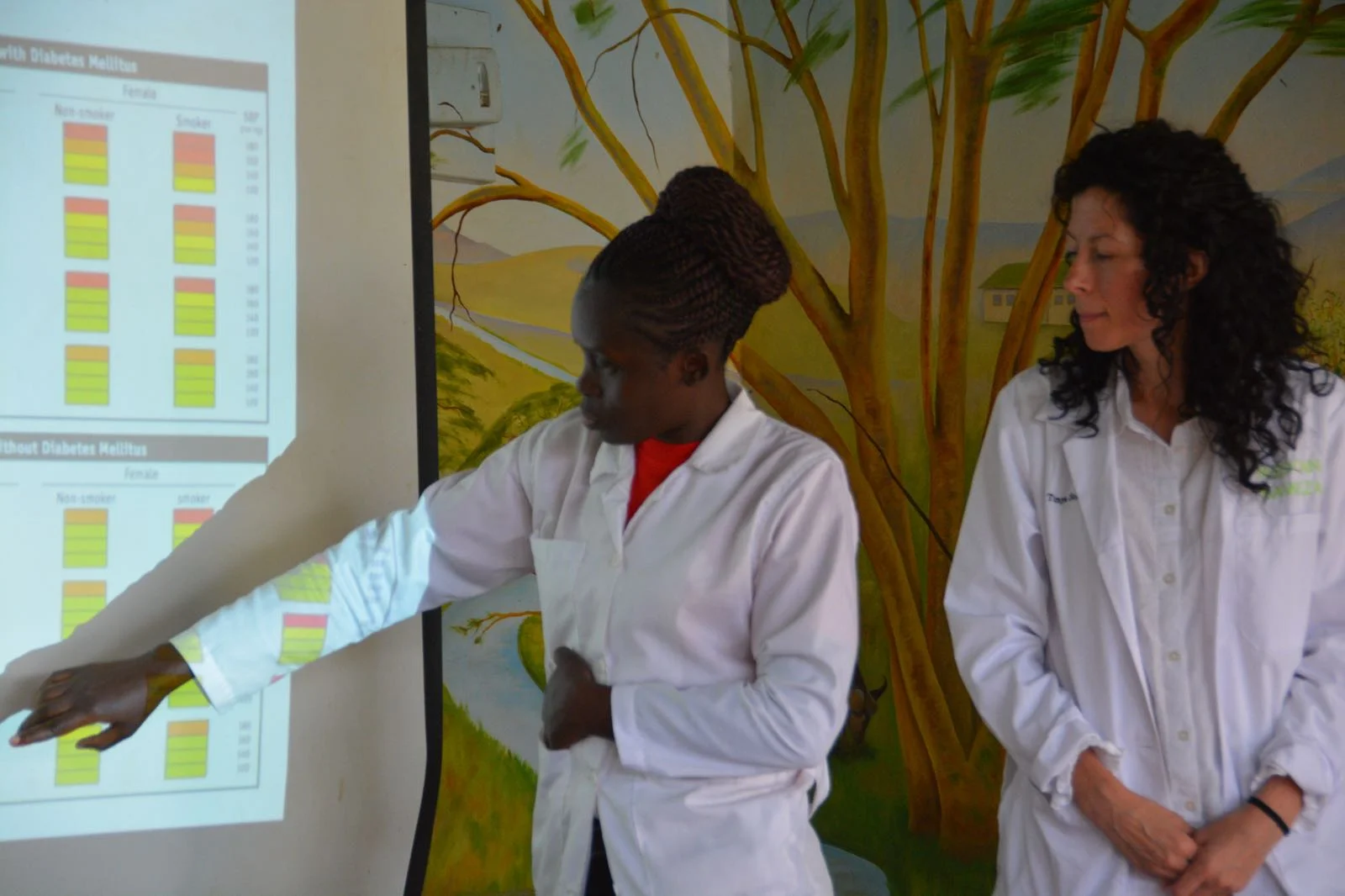
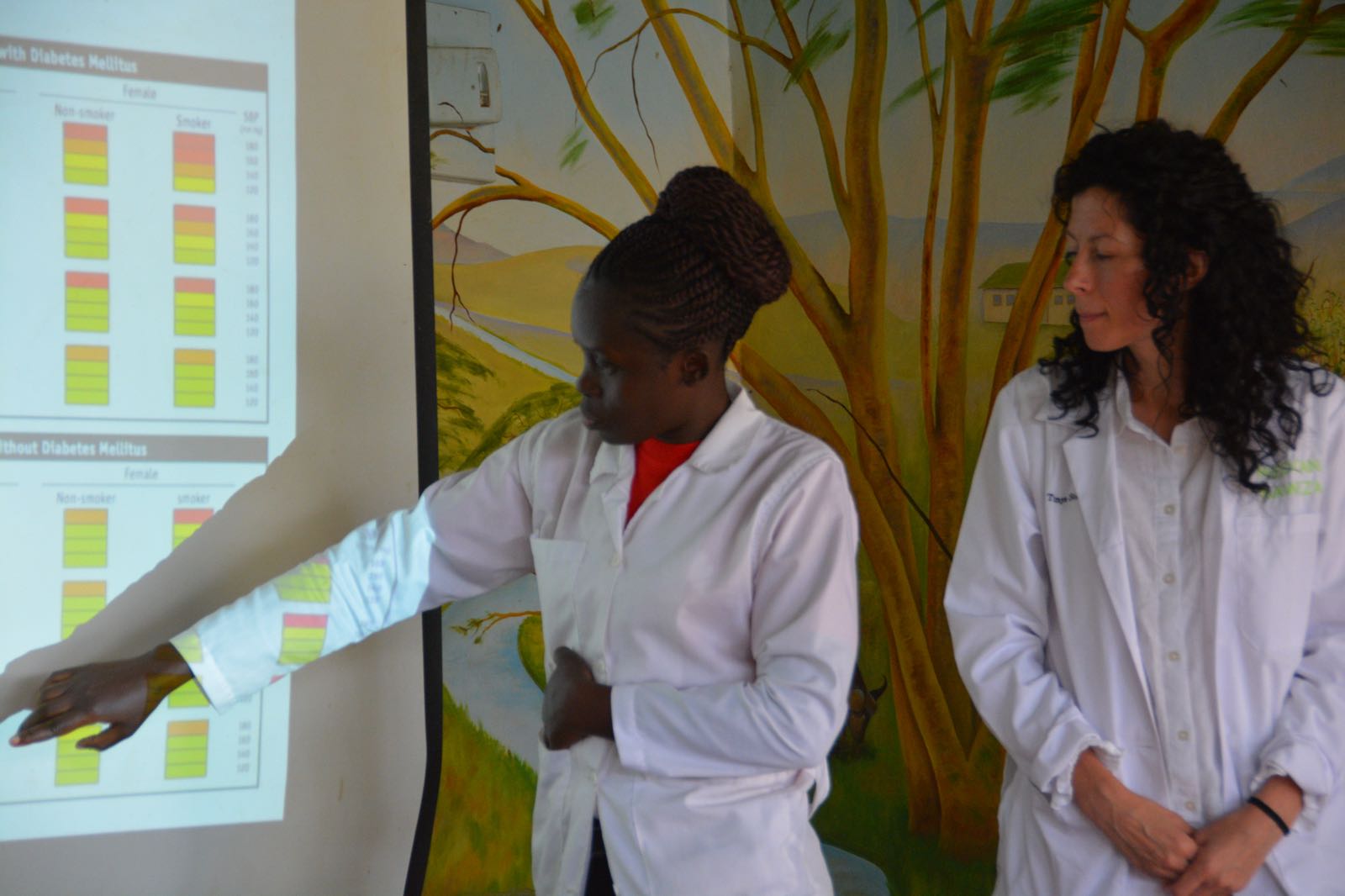
Dr. Tanya’s discussion was quite interactive, with several questions and references to cases that the nurses encounter at the clinic. They also had the opportunity to get up in front of their own peers and work through different scenarios of potential CVD patients. They needed to determine, based on certain data, which risk categories to put those patients into. Depending on the category, the patient will have a different treatment strategy. It was a good exercise not only to give the nurses a chance to demonstrate to their co-workers their own knowledge, but also was a stepping off point for a robust discussion on the nuances of cardiovascular disease cases and how you might navigate a particularly tricky scenario.

We were told that there has recently been a big increase in cases of malaria. Usually in a month’s time the clinic will see about 10 cases, but last month alone brought in 44 cases. This is mainly caused by the above average rainfall that the area has received. Good news for the animals and vegetation, but it doesn’t come without a cost. The stagnant water attracts the mosquitos and is where they like to breed. Fortunately the clinic has access to point of care diagnostics and can quickly determine if a patient presenting with a fever and other flu like symptoms has malaria, and if positive, commence immediate treatment with anti-malaria meds.
After a quick lunch, the team headed back to the clinic to see patients. Dr. Michael worked alongside one of the nurses providing training on the IMCI (Integrated Management of Childhood Illness) algorithm. This is an algorithm that can assist on when to give and withhold antibiotics. A child came in presenting with cough and cold symptoms and they were able to use the tool to determine that the patient did not in fact need antibiotics. Antibiotic stewardship, as well as managing the limited resources available to the clinic, are the ultimate goals. The nurses are too often inclined to give antibiotics to the patients when in fact it is unnecessary. This is mainly due to their uncertainty in the diagnosis and fear that they may get it wrong. The IMCI tool will hopefully give them confidence that they are in fact making the right decision and providing good care for their community.
One case in particular involved 2 young HIV+ boys. Unfortunately the boys had begun late on the antiretroviral agents (ARTs) and as well were not fully compliant on the drugs. By not taking the ARTs on a regular basis, their immune systems were compromised, resulting in warts developing on their face. Dr. Michael reinforced the importance of staying on the drugs in order to halt the progression of the warts and/or any other potential conditions caused by a depressed immune system.
Dr. Tanya worked with the nurse, Hagai. They saw several interesting patients including one woman who complained of knee pain when she squatted. Dr. Tanya thought it sounded like a condition called patella-femoral which normally would require a knee brace to help keep the knee cap in line. The interesting thing was the woman designed her own make-shift brace with a piece of gauze which she claimed made the pain subside, a design which Dr. Tanya thought actually resembled the brace you would normally get in Canada. The fact that she was able to intuitively put this together is sort of incredible if you think about it. But these are the kind of survival strategies that the community must employ in order to manage their health. Despite having access to the clinic, the woman’s ability to afford such a brace is limited. And the clinic’s access to such a brace is unlikely. So Tanya advised her to continue to wear the “brace” and teaches her how to do exercises that will help strengthen the area.
That’s it for now. Looking forward to another day of training and seeing patients tomorrow!
Thanks for reading!
Stacy ☺