Jambo!
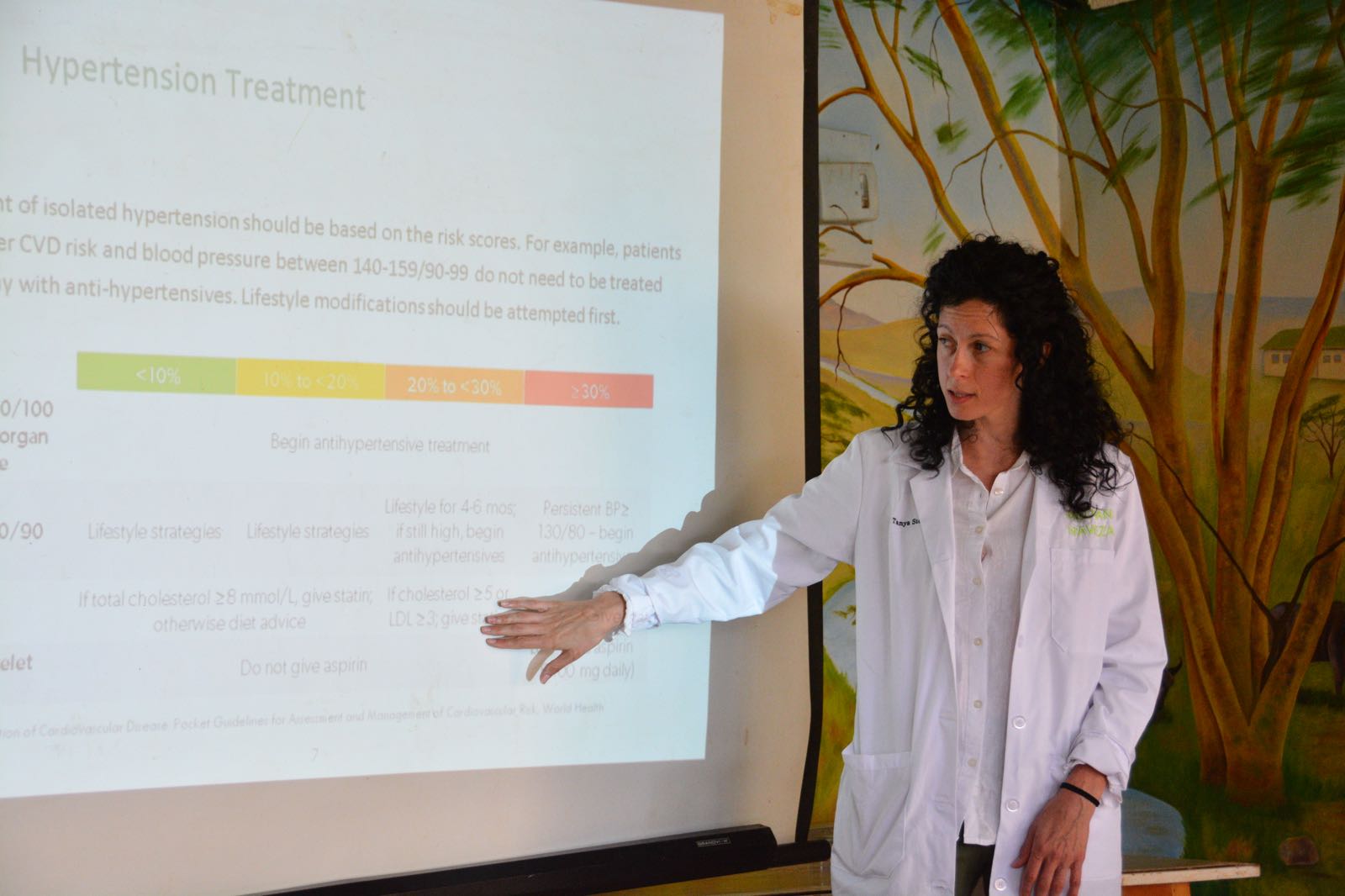
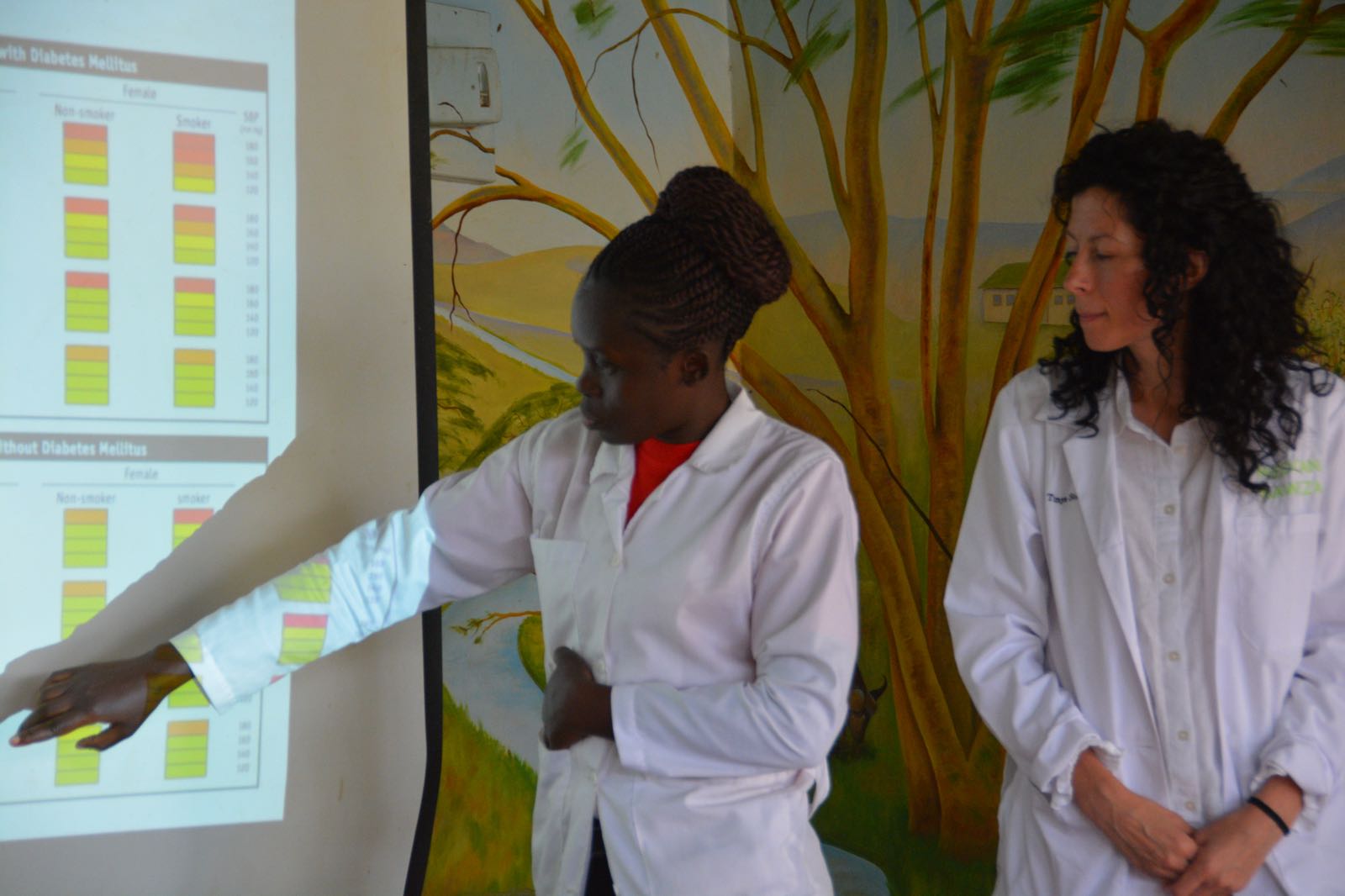
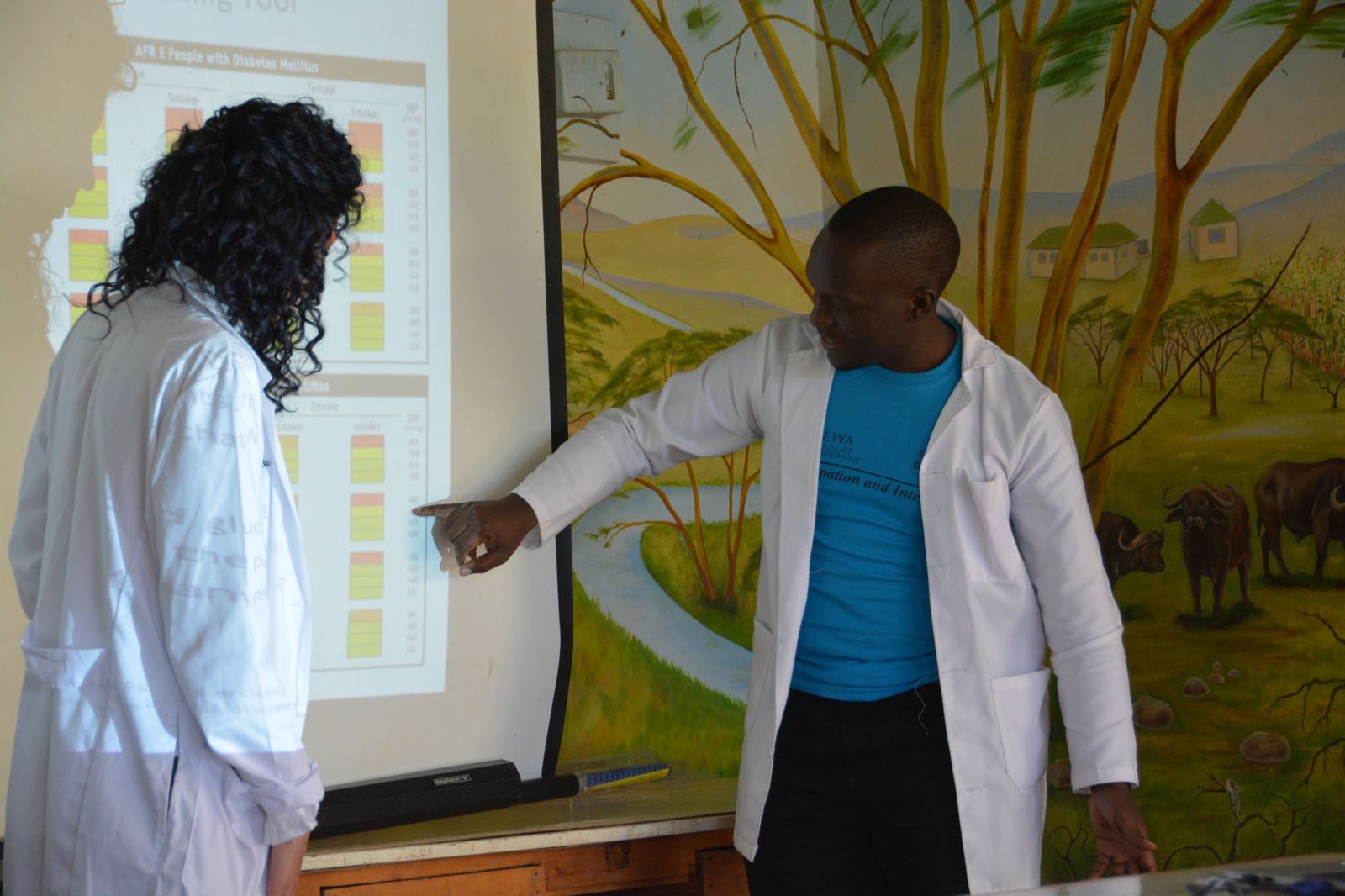
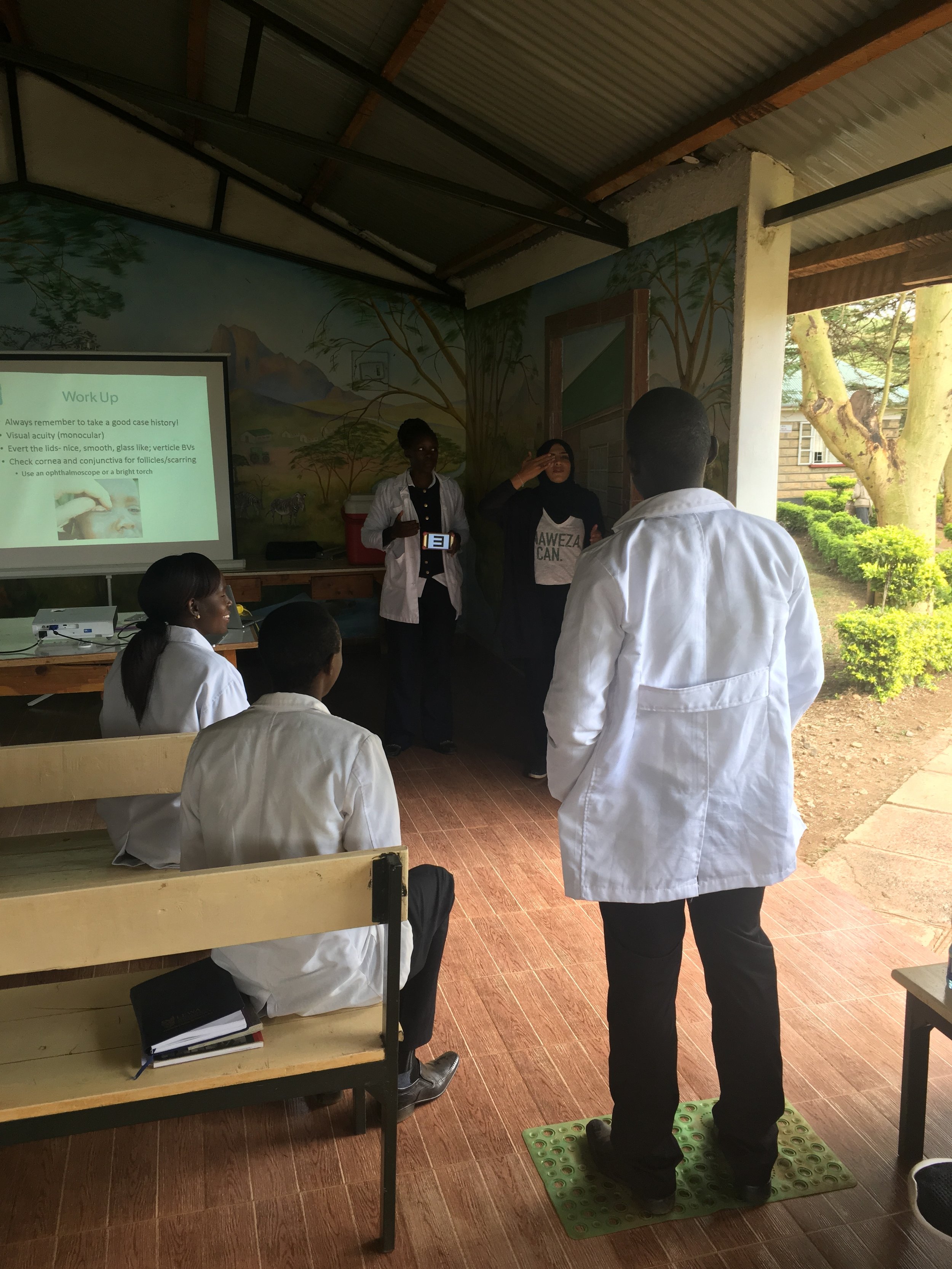
Our last morning at Lewa has arrived and we will be departing for Nairobi just after lunch. Hard to believe that our time here has come to an end. It’s been a fantastic trip once again, with the team making great strides on our Chronic Disease and Vision programs. The clinic staff seemed to be very receptive to all of the Continuing Medical Education sessions, asking many questions and absorbing as much knowledge from our doctors and nurses as possible in the short time we had with them.
We also made progress in solidifying our relationship with Lewa. We think it will be a fruitful partnership for many years to come for both of us. Our hope is to develop a template that we can take to clinics throughout the NRT, the consortium of about 30 conservancies in Kenya. Saving human lives and animal lives. It’s a good fit!
And of course, the best part of this trip for me is being part of a collective of people who come together to do something good simply because it’s the right thing to do. All of the doctors and nurses who support Naweza do so on a strictly volunteer basis. And although we feel privileged to stay in nice accommodation at Lewa, the days are long and hard. The doctors see complicated cases that many times they’ve learned about in medical school but have actually never witnessed in their practices. These are often illnesses and diseases that really only occur in rural, low-income settings. We try to provide some information prior to the trip, but nothing really prepares you for what you’re going to see. The access to testing is limited, so experience and intuition are many times all you have to go on.
Protocols, such as the one we use for our Chronic Disease screening program, help in these resource-limited locations. They use very simple criteria and are a good tool when out in the field going door to door doing active case detection. And it is simple enough that we can task-shift this job to a Community Health Worker, reaching more people for a fraction of the price.
So this is it. I’ve just spent the last 9 days with some of my favourite people in the world. Smart, funny, selfless, easy-going and with a sense of adventure. A special welcome to Dr. Tanya who did an amazing job teaching and training the local clinicians, always with a lovely energy and smile. Although she didn’t speak Swahili, she had an incredible way of connecting with them and the patients. And to Kristen, our nurse; when she was not assisting the doctors, being a model for abdominal exam teaching sessions (thank you!), or giving presentations, she was our official bug killer. She might be the bravest Naweza family member ever!
Our next trip is planned for January 7 to 17th. We will continue with our work on the EMR, hopefully launching it in January. Danet, our IT person, worked on it with Dr. Michael and Jen throughout the week and has made good progress, but there is still more to do and we want to get it right before presenting it to the clinic.
So until then, thank you for reading. And don’t forget to keep up with us on Instagram (@medcannaweza) and Facebook. We’ll continue to update throughout the year on our progress and share our many photos we’ve all taken, capturing the many moments together as we help this special community.
With best wishes,
Stacy ☺