Jambo!
It’s our final morning waking up at Ngiri House, our home for the last 7 days. Rose and her staff have taken such good care of us, providing beautiful meals, doing our laundry, organizing transportation and basically anything else that we need.
Dr. Sue pointing at the elephants in the background. Earlier Sue and Sidiqa joined me in my regular workout and this is our daily view
daily visitors of monkeys and impalas as we work, eat or exercise
Family of monkeys eating some snacks from our front lawn at Ngiri House
Sidiqa and Sue joined me for our daily circuit workout (thank god for the 7-minute workout app) that we do outside overlooking the plains of Lewa which was full of impala, elephants, zebras, monkeys, warthogs and many more magical creatures to keep us company. The setting is truly surreal and our sense of gratitude for being there couldn’t be stronger.
Dr. Michael examining a young patient at yesterday's outreach
A mother and resting child speak to Dr. Michael during yesterday's outreach
During breakfast we had a lovely surprise visit from the clinic staff to come and say one last goodbye. They have a tradition of guests signing their visitor book. So each of us wrote a personal message thanking them for a great visit. Again we had some laughs about the week. One of my stories involved a mother who had brought her baby in to see Dr. Michael. Her baby had become fussy during the visit and she was trying to bounce him and hold him in different positions, but to no avail. He kept crying. All the while she kept smiling as she discussed the baby’s symptoms with Michael, never losing her composure. I just marveled at the way she kept calm despite the baby’s obvious displeasure! She then without missing a beat bent over from the waist, thrust the baby on her back and then threw a type of sarong around the baby and secured it by tying it around her chest. Although better, he still wasn’t quite settled. Mind you, she is continuing her discussion with Michael at this point. And yes, still smiling. I on the other hand was sweating just watching her, and wanted to help, but realized I was way out of my league. For her final and decisive move, she slid the baby under her arm and then back up the front so that his little head rested on her chest. And he finally fell fast asleep. It was nothing short of masterful.
All of the staff laughed and said how this was quite common. And John, the ambulance driver then demonstrated how everyone in fact is very good at balancing things on their head while they carry many things in their hands. So he demonstrated putting his phone on his head and began walking around, bending over, all the while with the phone lying completely still on his head. All I could think was how is it possible that he do this and I can’t even keep my own phone from falling out of my pocket!
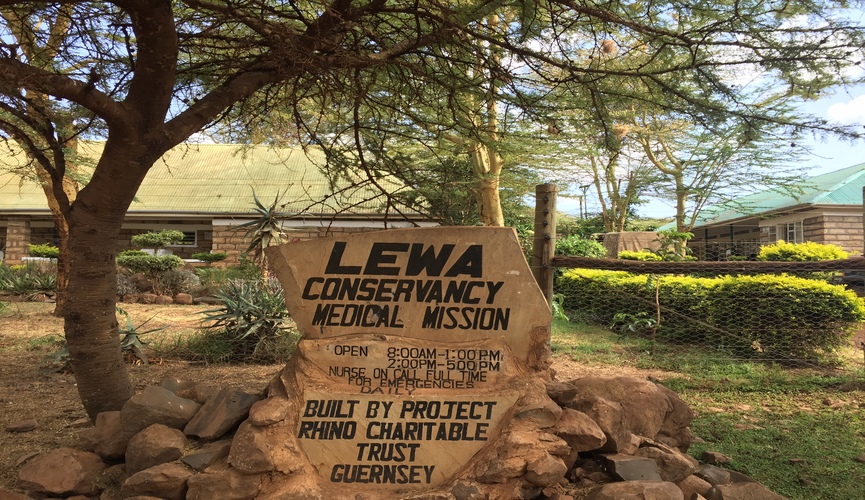
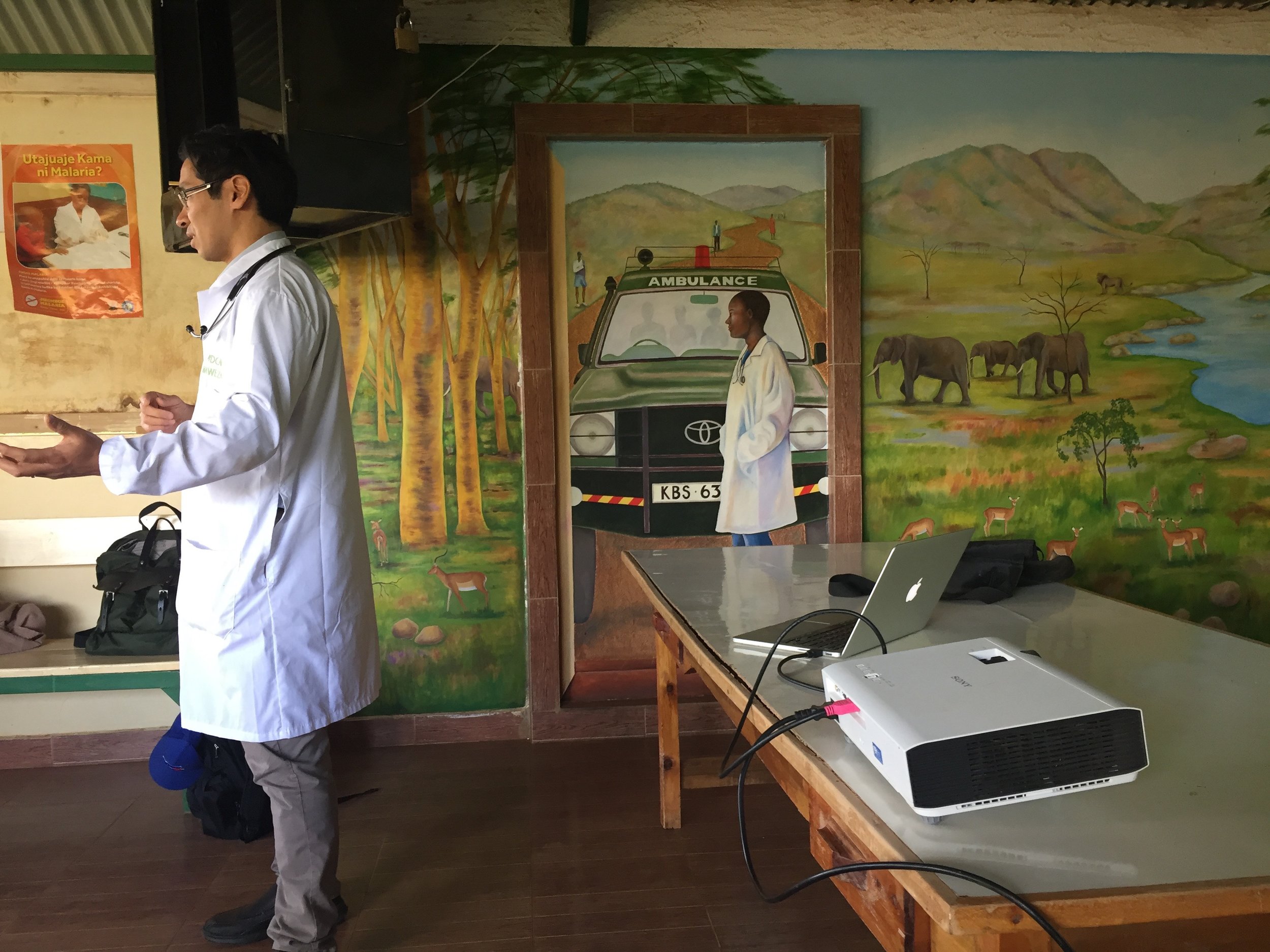
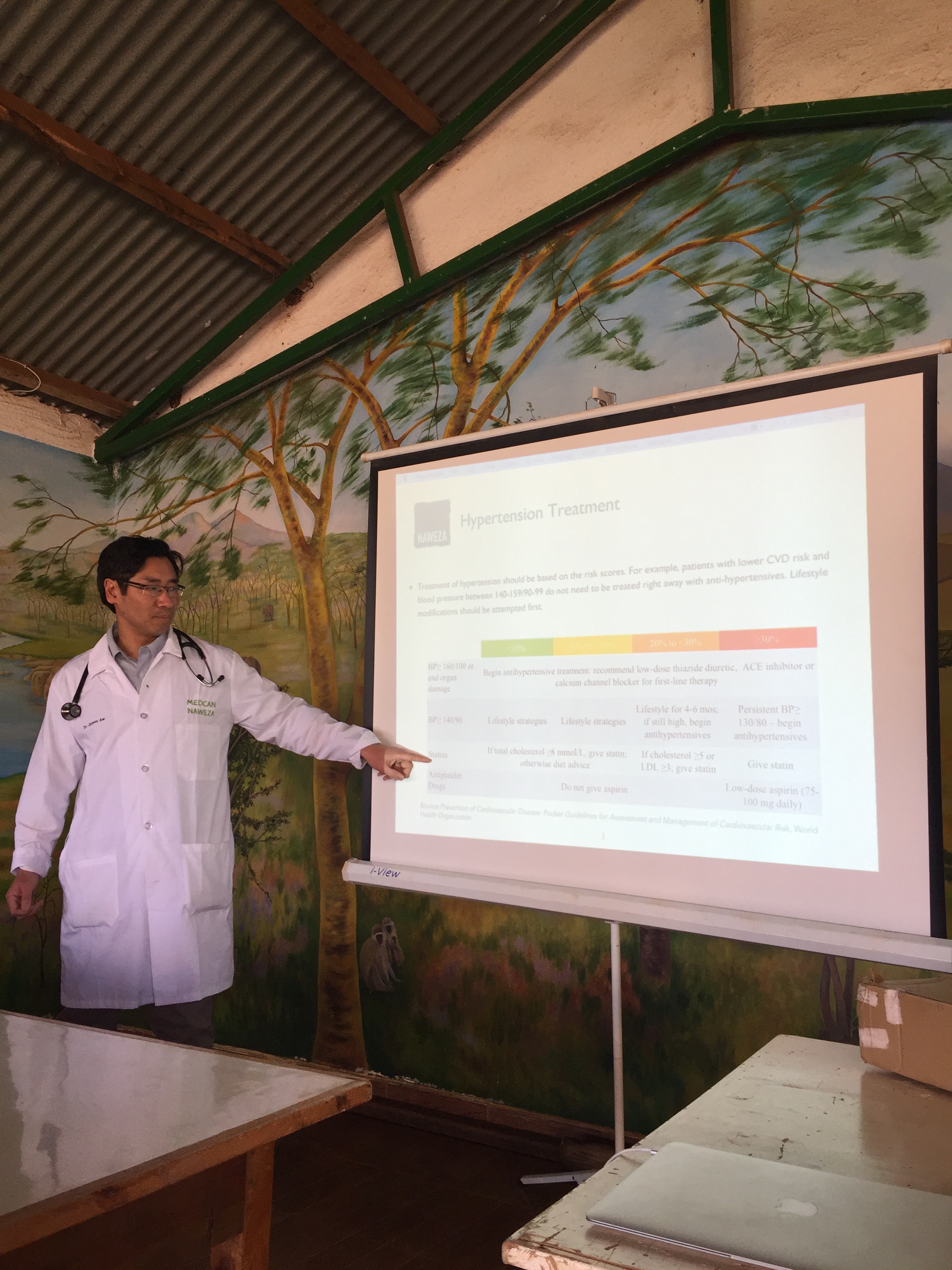
But it was this easy exchange and dynamic that we feel so grateful to have with the staff. We work hard, have high expectations, challenge them during CME and clinic sessions, constantly putting them on the spot for correct diagnoses and treatment strategies, but always with respect and kindness. These are nurses who are being forced to be doctors in order to care for their community. That’s quite a bit of pressure and we know that is not an easy ask. But their people are relying on them and we want them to know that we are there to help provide the training and knowledge to hopefully close the gap if just a little bit.
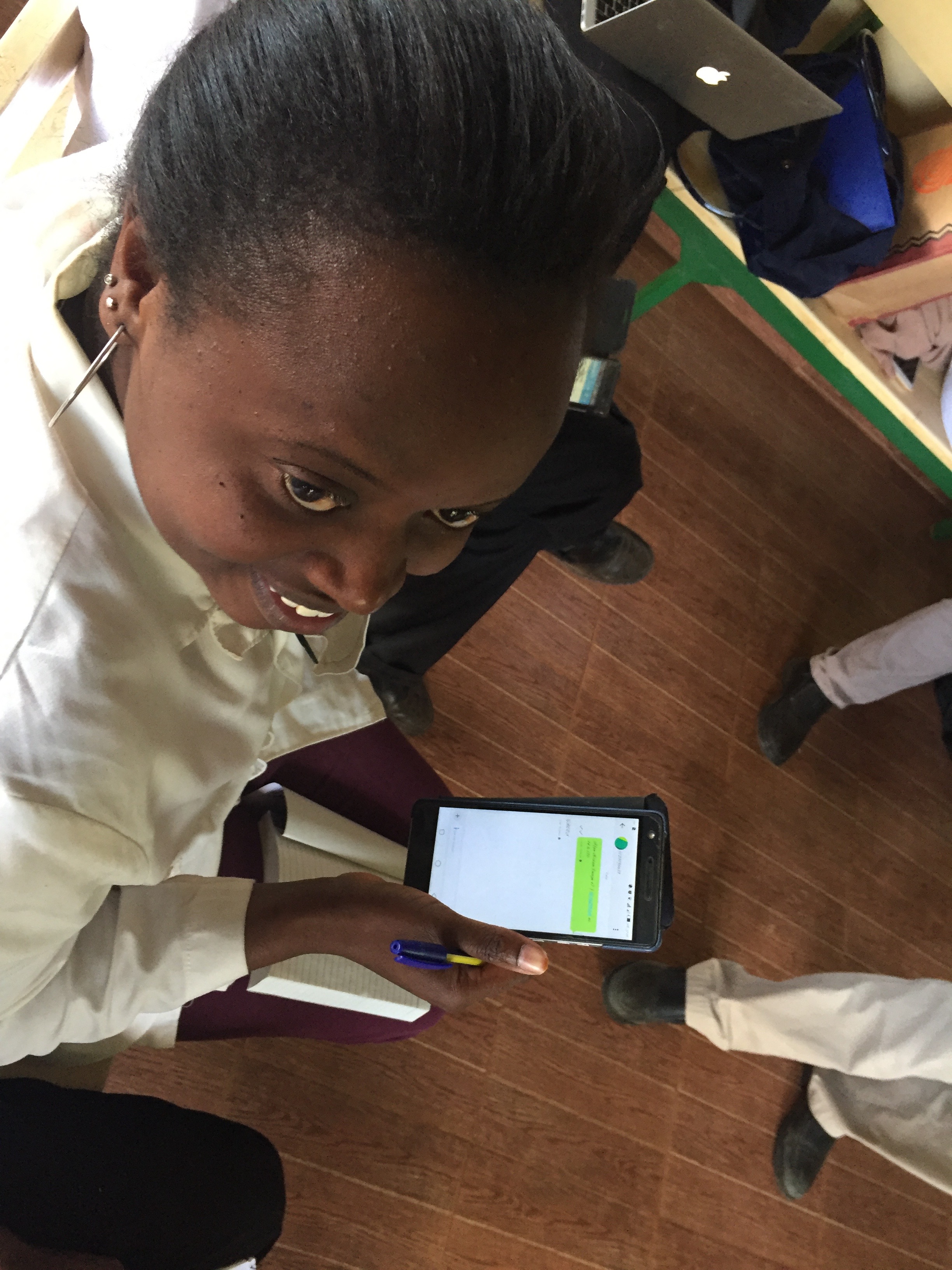
Dr. Paul Cohen, a dermatologist at Medcan, pictured here with local children during his first Naweza trip in July 2016. During the February 2018 trip, he supported Medcan Naweza from Toronto via the WhatsApp chat group we created.
One of our new strategies in ensuring a line of communication between us and the clinic is our new WhatsApp chat group. The clinic will now use the chat group for any complicated cases that they encounter, enabling the Medcan Naweza docs to respond and provide timely guidance. In fact during our Outreach we had a dermatology question and we sent a photo of a rash to Dr. Paul Cohen who has been on a previous trip. Within minutes Dr. Paul responded with potential diagnoses, things to check for and recommended treatment strategies. Technology is going to allow us to have more impact with our programs. Especially as Kenya continues to improve infrastructure and connectivity, which I have seen over the last 5 years since we began this initiative. Things are looking bright!
After the flight we return to the other wild part of Kenya - the Nairobi streets.
We then headed to the airstrip, gave a big hug to our driver Benjamin who has been so patient and attentive to us this past week. And we boarded our plane to Nairobi, a (very) bumpy 40-minute ride.
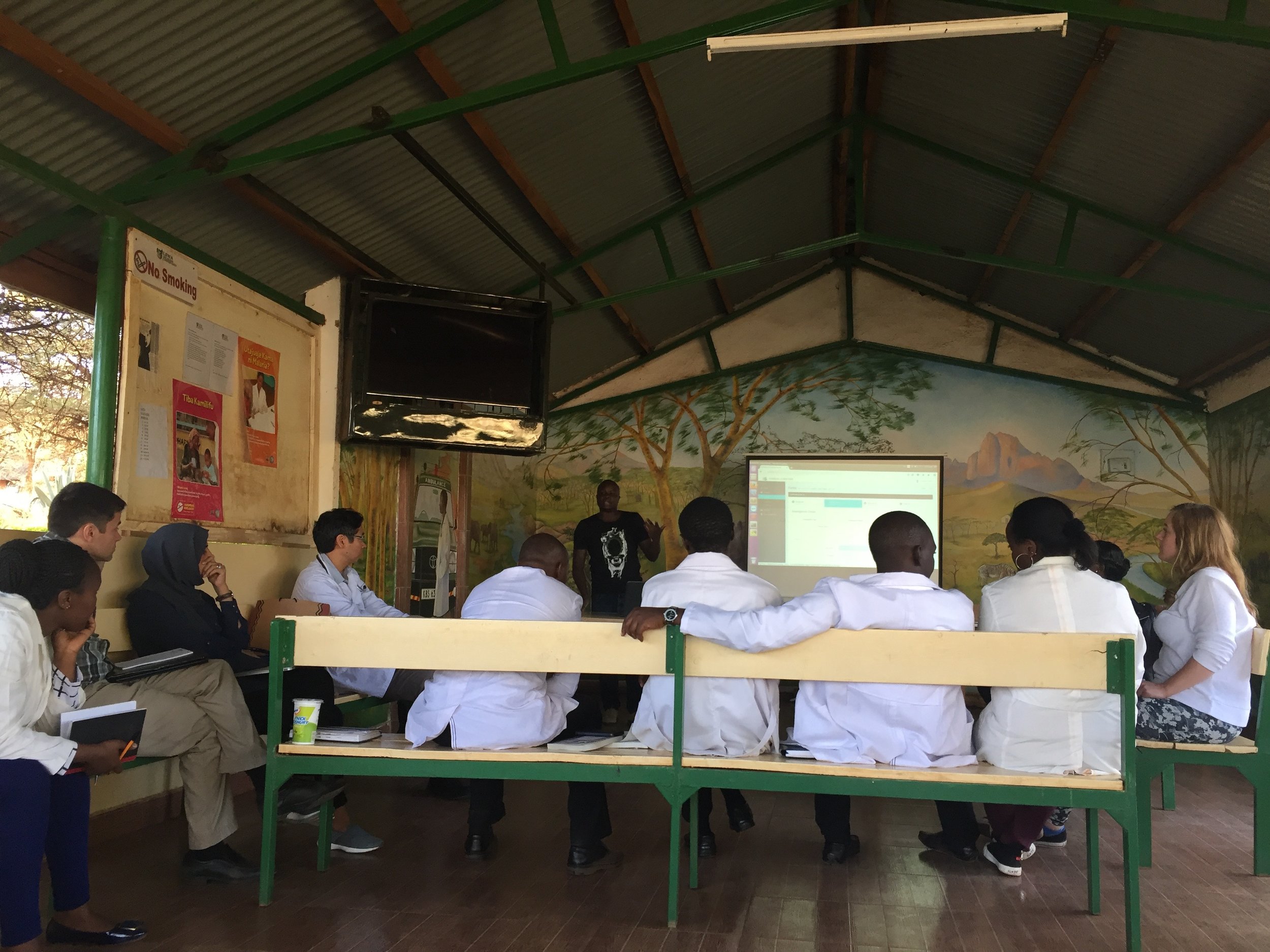
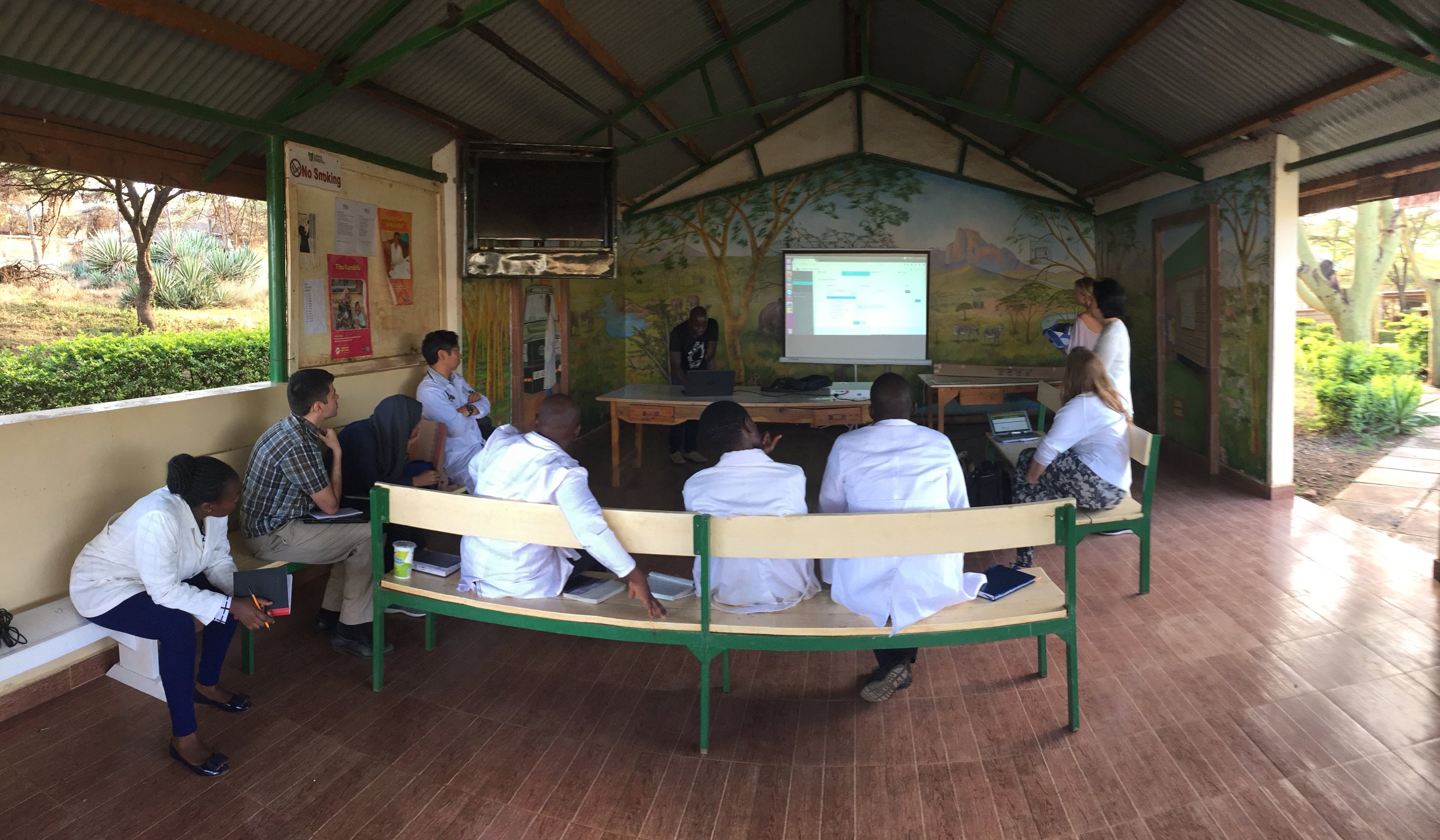
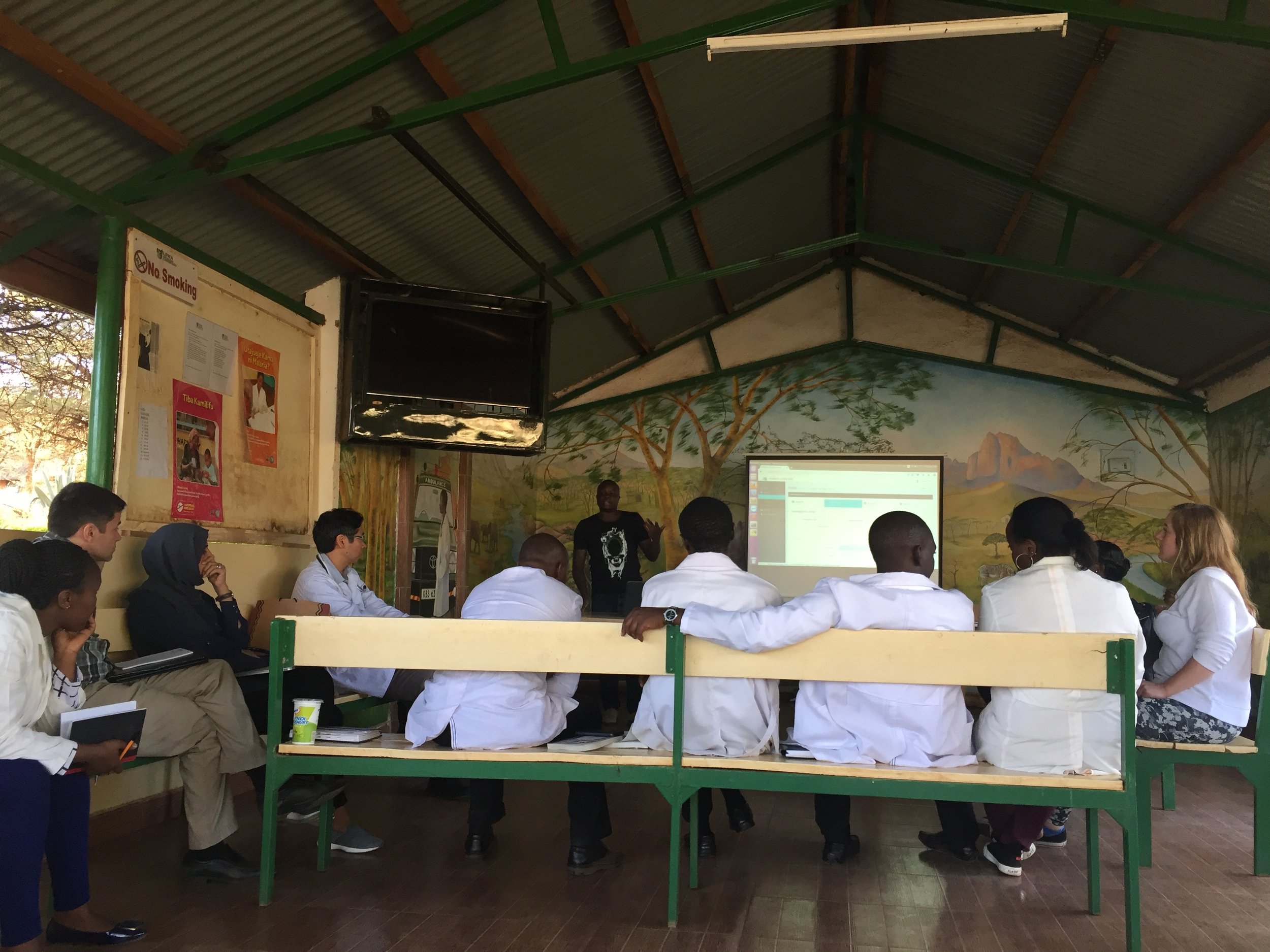
Over lunch we discussed next trip dates, hopefully July and Jan/Feb and the steps going forward. Our main tactical goal will be to operationalize the EMR. Although the government-issued EMR system that they currently use is quite comprehensive, it does not include most of the data points that we need to properly manage the patients in our Chronic Disease Program. It is for this reason we were forced to build our own. In one month we will see the next iteration of it and hopefully it will be ready for a soft launch. Danet, the builder of the EMR would then go back to Lewa and begin installation, testing and training. And as any EMR system, it won’t be easy. But we’ve kept the program purposely simple to help mitigate the inevitable complications, with the long term plan of building onto it and integrating it with the Clinic’s current system.
So this is it for now. It has been an incredible journey this week.
- We’ve made strides in our Chronic Disease Program
- Have buy-in from the CEO of Lewa
- Continued training in women’s health and family planning
- Continued training in optometry and will be doing a vision clinic at a school of 500 providing prescription glasses to those in need, and lastly
- Have increased community engagement by a tremendous amount by conducting interviews of the community and clinic staff as well as talks on health education.
All round a very fruitful trip, which has left us energized and excited to get on with it and really try to make a difference by equipping this amazing community with the tools it needs to keep its beautiful people healthy.
Once again, thank you for reading. Please continue to follow us on Instagram https://www.instagram.com/medcannaweza/
If you'd like to see a sneak preview of some of the footage that you'll see there over the coming months, check out this "trailer"
We’ll keep posting the photos from the trip throughout the year to keep you updated on our progress.
Until July, with best wishes,
Stacy :)